Clear Guidance. Skilled Hands. A Caring Team You Can Trust.
TRUE SMILE Dental Centre Al Reem Island
When a tooth is too damaged to save, or if it’s interfering with your health or treatment, removing it may be the best option. At TRUE SMILE Dental Centre, we handle everything from straightforward extractions to complex oral surgeries with calm professionalism and a patient-first mindset.
We help patients move forward, with less pain, fewer complications, and a clear understanding of every step.
When Is Tooth Removal the Right Choice?
Tooth extraction is never our first option, but sometimes it’s the only one that truly protects your oral health.
You might need a tooth removed if:
- It’s badly decayed or cracked beyond repair
- It’s loose from advanced gum disease
- It’s impacted or growing in the wrong place
- It’s causing pain, crowding, or infection
- It’s blocking orthodontic or implant treatment
We also regularly perform emergency tooth removal for patients with sudden infections or injuries. Whether you need urgent relief or surgical planning for a complex case, our team is ready to help.
Our Services
At TRUE SMILE, we provide a wide range of extraction procedures, from routine to highly specialised.
General Tooth Extractions
For visible teeth with accessible roots, we often recommend a simple tooth extraction under local anaesthesia. This includes molars, loosened teeth, or extractions before orthodontic work. Most patients go home the same day with mild discomfort and rapid healing.
We’re also one of the few clinics in the area to offer same-day tooth removal in Abu Dhabi when needed, especially in emergencies.
Surgical Extractions: Precision When It Matters
Some teeth can’t be removed without surgical access. That’s when we perform complex tooth extractions using sterile microsurgical tools, gentle bone reshaping, and careful planning to protect surrounding structures.
This applies to:
- Teeth broken at the gumline
- Curved or multiple roots
- Teeth trapped under gum and bone
- Failed root canal cases
These cases are handled by our surgical dentists in Abu Dhabi, who specialise in minor oral surgery. We use 3D imaging, custom sedation plans, and post-op support for the safest experience possible.
Wisdom Teeth: Timing and Technique Make the Difference
Wisdom teeth are the most commonly removed teeth for a reason. They often lack space to grow, erupt in awkward directions, or become trapped in the jawbone, causing pain, swelling, infections, or damage to nearby teeth.
We regularly perform:
- Surgical wisdom tooth extraction in Abu Dhabi
- Lower and upper wisdom teeth removals
- Impacted third molar surgeries under sedation
Every case starts with imaging. For example, if a wisdom tooth lies close to the nerve, we might adjust our technique or stage the extraction to reduce risk.
Impacted, Ectopic, and Extra Teeth
Some teeth erupt in places they shouldn’t, like the roof of the mouth or deep behind the molars. Others never erupt at all, staying buried and risking infections or crowding.
If you or your child have been told a tooth is “hiding” or “in the wrong place,” it may be:
- An impacted canine
- A supernumerary (extra) incisor
- A misplaced premolar
- Or even a tooth inside the sinus area
We manage these with ectopic tooth removal, impacted tooth surgery, or referrals for orthodontic guidance when the tooth can be saved. In one case, an 11-year-old girl had a canine pressing against the roots of her front tooth. We safely removed it and coordinated with her orthodontist for future alignment.
Root Fragments, Retained Roots & Fractured Roots
Sometimes, what’s left behind is just as important as what’s removed.
A patient recently came to us after a previous clinic attempted an extraction that left the root behind. She had constant discomfort and swelling. Through a root fragment removal surgery, we carefully accessed and lifted the piece without additional bone damage. She was symptom-free within the week.
We handle all types of retained root cases using gentle, controlled techniques and appropriate anaesthesia.
Apicoectomy (Root-End Surgery)
When a root canal fails, but the tooth is otherwise worth saving, we may suggest an apicoectomy. This procedure removes the infected tip of the root and seals the area to prevent recurrence. It’s a form of endodontic surgery that’s highly effective when traditional treatments have failed.
It’s especially useful for molars with prior root canals or teeth with chronic abscesses that don’t heal despite antibiotics.
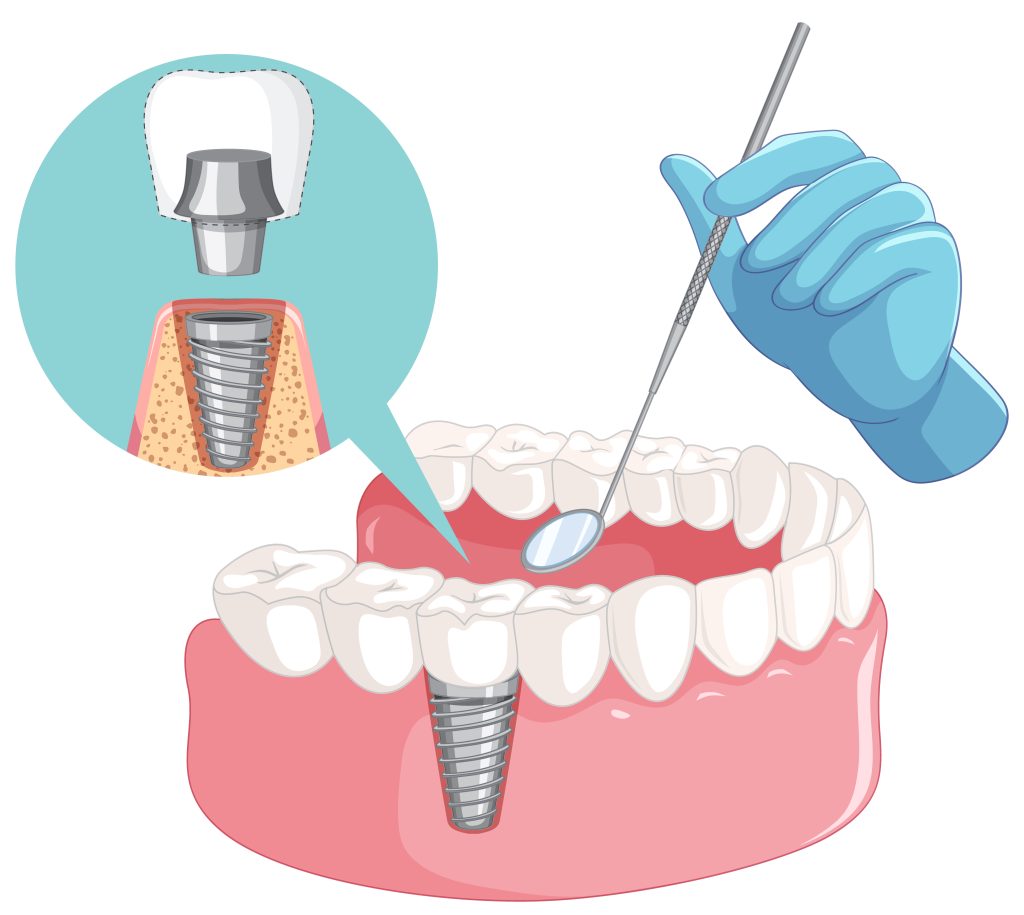
Socket Preservation, Bone Grafting & Sinus Lift
After a tooth is extracted, especially a molar or premolar, we may recommend additional treatment to protect the surrounding bone:
- Socket preservation grafts help maintain the ridge shape
- Alveoloplasty smooths bone for future dentures
- Sinus lifts with bone grafting create space for upper molar implants
- Bone regeneration procedures prepare the area for implant placement later
All of these support better long-term outcomes and preserve your options for future care.
What to Expect: Before, During, and After Your Extraction
Before:
You’ll receive a detailed consultation, panoramic X-ray, and CBCT scan if needed. We’ll review your medical history, medications, and tailor your anaesthesia plan.
During:
Extractions are performed in a sterile setting by an experienced clinician. Surgical cases may involve small incisions, bone removal, or tooth sectioning. Most are completed in under an hour.
After:
You’ll be given detailed post-op instructions and follow-up. Most patients return to work or school within 2 to 3 days, with full healing of soft tissue in 1 to 2 weeks and bone healing in 6 to 8 weeks.